
It is a well-known fact that the pandemic of COVID-19 can be controlled only by boosting the production of antibodies in the immune system of patients. However, a recent article in Nature magazine reports otherwise. According to scientists at Yale University, the immune system of patients with severe COVID-19 is impaired significantly and boosting the production of antibodies cannot really control the illness.
Diseases like lupus and rheumatoid arthritis are autoimmune disorders, which are treated by boosting the production of autoantibodies. These antibodies interact and target damaged tissues associated with autoimmune diseases. In patients afflicted with COVID-19, autoantibodies target multiple organ systems that are otherwise healthy. This means that healthy tissues in the brain, liver, and gastrointestinal tract are attacked by autoantibodies. Moreover, they also target blood vessels and platelets in the bloodstream. This implies that the severity of COVID-19 is directly proportional to the number of detected autoantibodies.
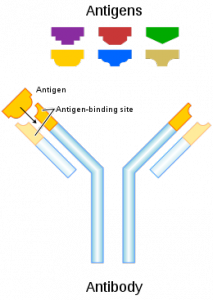
Scientists at Yale University also found out that these autoantibodies attack many proteins in the immune system, that is, proteins that otherwise effectively fight infections are damaged by autoantibodies. Therefore, the situation is like a double-edged sword in patients with severe COVID-19 infection. In general, antibodies are effective in combating infection, but when COVID-19 infection is severe, patients develop autoantibodies. These autoantibodies attack multiple types of cells and tissues.
In most cases of COVID-19, the infection became severe and led to the production of autoantibodies, which are antibodies that caused extensive damage. However, it must be noted that in most severe cases of COVID-19, patients already had a pre-existing disease that caused the production of autoantibodies. The observation was done after testing mice with pre-existing autoimmune disorders and who had developed COVID-19 infection. Such mice had a large concentration of autoantibodies. Such kind of sickly mice were more likely to succumb to COVID-19 infection as there is no effective cure till date.
Autoantibodies are also called rogue antibodies and are believed to be existing for a long period of time in patients with pre-existing autoimmune disorders. When such patients contracted COVID-19 infection, they developed severe form of the disease that could not be tackled with existing medications and injections. The medical symptoms of COVID-19 became severe and long lasting in these patients. In other words, the virus became a legacy in the bodies of these patients. Therefore, all patients with autoimmune disorder should immediately be vaccinated to prevent more cases of severe COVID-19.
In patients with autoimmune disorder, autoantibodies are produced even at a mild stage of COVID-19 infection. The study was conducted by an esteemed team of scientists and physicians working at Yale University. In their clinical practice, they made concerted efforts to tackle COVID-19 infection: they screened blood samples of 194 patients with COVID-19 infection; the extent of severity was different in different patients. Nevertheless, autoantibodies were detected in all the blood samples of these patients.
Yale scientists developed a novel technology to detect the extent of damage caused by autoantibodies to proteins of the immune system. The technology was named Rapid Extracellular Antigen Profiling (REAP), and it explored the interaction of autoantibodies with approximately 3,000 proteins of the human body.
The scientists at Yale believe that the study’s findings may be used to develop novel strategies to combat or even prevent the damage caused by autoantibodies in patients with severe infection of COVID-19. Moreover, REAP technology is not just restricted to measuring the response of autoantibodies to COVID-19 infection.
The technology can be used to determine the damage caused by autoantibodies in patients with many types of autoimmune disorders and chronic diseases. These scientists are now exploring whether the technology can be used to determine the damage caused by autoantibodies in cancer patients and in patients with neurological disorders.

