A preclinical study was conducted to treat the most common form of brain cancer in humans, that is, glioblastoma. This experimental study was conducted by researchers at the University of Texas at Dallas and the UT Southwestern Medical Center. They have developed a novel technique that delivers medication through the barrier between the bloodstream and the brain. The research study was performed on mice and published in Nature Communications magazine.
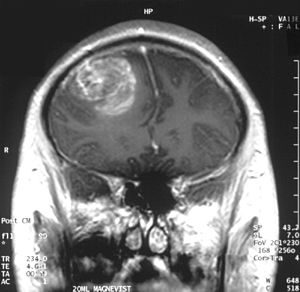
In the USA, the most aggressive form of brain cancer is glioblastoma. Every year, about 12000 patients are diagnosed with glioblastoma in the US. The average survival rate of these patients is just 15 to 18 months, post-diagnosis. Presently, the conventional modes of treatment, such as chemotherapy, radiation, and surgery, are not really effective in most cases. Most chemotherapeutic agents cannot pass through the blood-brain barrier, making them ineffective in destroying glioblastoma tumors.
The primary function of the blood-brain barrier is to restrict and prevent substances from the bloodstream from entering the parenchyma in the brain. The blood-brain barrier shows high selectivity as a filter and acts a protective barrier in the human brain. The blood-brain barrier is the biggest hindrance in the treatment of any disease related to the brain. Although it is just 1 micron in thickness, it obstructs about 98% molecules from entering the brain.
Our current research study was conducted on experimental mice, which were engineered genetically to contain mutations of human glioblastoma. The researchers used gold nanoparticles to co-deliver medication and to target the blood vessels. The nanoparticles were administered through an injection in the bloodstream. When they reached the mouse skull, they were activated with non-invasive laser pulses.
Owing to laser treatment, thermomechanical waves were formed in the brain of mouse model. The blood-brain barrier became permeable within a short span of time, thereby enabling the medication to enter the target area. In this experiment, researchers used a chemotherapeutic drug named paclitaxel. This drug is usually used to treat ovarian, lung, and breast cancers. On its own, the drug molecule fails as it cannot surpass the blood-brain barrier in patients with brain cancer.
As the novel drug delivery method could permeate through the barrier, the technique was successful. The size of the brain tumour shrank in size; the overall survival rate of experimental mice was more than 50%. These preclinical procedures need to be guided by further research studies on humans. This is a novel mode of treating diseases like brain cancer, offering hope to patients with high mortality.
