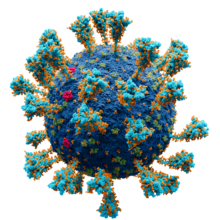
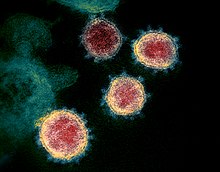
Although developed countries have now relaxed the rules of lockdown, the pandemic of COVID-19 is now complicated with an even more severe infection of SARS-CoV-2. This infection would have impeded the bounce back to normal life had there been no effective drugs to control the situation. However, this significant threat is now averted by some breakthroughs in recent research studies. Scientists have developed a combination of drugs named Nafamostat and Pegasys to control the pandemic. They are easy to use, effective, and fulfill the criteria of availability.
Laboratory synthesis of combination drugs
The combination of drugs named Nafamostat and Pegasys were quite effective in suppressing the life-threatening infection of SARS-CoV-2. These drugs were tested at the Department of Clinical and Molecular Medicine, Norweigan University of Science and Technology. A special cell culture was prepared to perform this experiment. The results indicated that the combination of drugs were quite effective, indicating that it is fit for human consumption.
Currently, COVID-19 infection is being controlled by administering monotherapy of Nafamostat. The efficacy of this drug is being extensively tested in laboratories of Japan and other Asian countries. Erstwhile, Pegasys was used to treat patients with hepatitis C. A combination of these two drugs seemed to have a positive impact on patients suffering from SARS-CoV-2 infection.
There is a factor named TMPRSS2 in our cells. It causes the replication of SARS-CoV-2 virus in cells. The combination drugs of Nafamostat and Pegasys effectively attacks this factor in cells, according to a leading professor of molecular biology at the laboratory. This observation has become a major good news for researchers who are determining how effective is Nafamostat drug against COVID-19 infection.
A low dosage of combination drugs is needed against SARS-CoV-2 infection
The combination of Nafamostat and Pegasys drug is needed to low doses to tackle the serious infection of SARS-CoV-2. Not only has the clinical outcome of patients been positive, the side-effects of this combination therapy been minimum. These clinical advantages have been highlighted by a leading researcher at the laboratory. Although the combination of drugs is not cheap, it is indeed quite inexpensive. Thus, these life-saving drugs can be rendered to patients infected with SARS-CoV-2 all across the world. The only limitation is the fact that Pegasys drug is quite costly.
Scientists all across the world are working hard in the fight against COVID-19 pandemic, which has caused 4.55 million deaths all across the world. Moreover, there are many remote areas in this world where the cause of death is not known accurately, leading to a growing number of deaths unreported. Although an international team of researchers worked at the laboratory, the cohort of patients was only from Norway.


