Drugs that are active epigenetically would help a cell in reading the parts of a genome. These parts were either blocked earlier or inaccessible to the cells of the human body. Thus, new mRNA transcripts and proteins can be formed. This important finding has been presented by scientists of the German Cancer Research Center and the University Hospital of Tubingen.
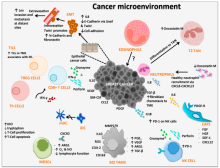
The immune system would be able to identify cancer cells, thanks to the activity of “therapy-induced epitopes.” Immunotherapies are now being provided to treat patients with different types of cancer. But, all the cancer patients do not benefit from immunotherapy. The treatment fails in some cases because the immune system of the patient is not able to identify cancer cells.
Antigens are protein structures, which are transported by cancer cells onto their surface. At this stage, the T cells of the immune system recognize and differentiate them from healthy cells in the human body. In such cases, immunotherapy is effective and successful.
The antigens can be proteins associated with cancer, and they are also known as tumor-associated antigens. Antigens could also be proteins that have been modified by mutations. They are known as completely new gene products. These products are formed in tumor cells when completely new areas of the genes are being read.
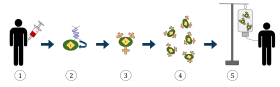
Researchers of this study decided to make the immune system quite visible to cancer cells. The cells were equipped with completely new antigens. This was possible due to the help offered by cancer drugs, which were epigenetically active. Many cancer patients are prescribed such types of drugs. The epigenetic markers of the DNA or the proteins associated with the DNA are subjected to these drugs.
Thanks to the epigenetic markers, researchers could determine whether certain parts of the ist genome in mRNA could be translated by cancer cells. Decitabine or the HDAC inhibitors are a class of demethylating drugs, which have epigenetic effect. They help in reading those parts of the genome, which were either blocked or were inaccessible earlier. Thus, new mRNA transcripts can be created in the cells.
In this study, a lung cancer cell line was treated with decitabine and HDAC inhibitor in a culture dish. This induced the formation of several new transcripts, which were detected by RNA analysis. The origin of most of the new transcripts could be traced to endogenous retroviruses. The sequences of these transcripts accounted for upto 8% of the human genome, so they were considered as relics of retroviral infections.
In general, epigenetic mechanisms block their transcription. In cancer cells, the effect of the neoepitopes is much stronger than that in healthy cells. These neoepitopes are induced by Decibtabine and HDAC inhibitors. Cancer cells have high proliferation rate. The researchers now had to determine whether the therapy-induced transcripts could be used for coding segments of immunogenic proteins, that is, peptides.
Mass spectrometry was used for analysis in this study. The researchers were able to identify 45 neoepitopes, which were present on the surface of cancer cells post-treatment. The results obtained were reproducible with a large number of different cancer cell lines. In the culture dish, the cytotoxic T cells could be activated by therapy-induced neoepitopes.

