
Molnupiravir is the world’s first antiviral medication in the oral form. This medication has been approved for treating COVID-19 patients who have developed mild to moderate symptoms. This medication is safe for use only in adults who have been tested positive for COVID-19 and who have atleast one underlying disorder that poses as a risk factor. Molnupiravir has been jointly developed by Merck and Ridgeback Biotherapeutics. In the United Kingdom, the medication has been approved for use by the United Kingdom Medicines and Healthcare Products Regulatory Agency (MHRA). Merck has now requested United States Food and Drug Administration (FDA) to authorize the use of molnupiravir in the US.
Merck would also be filing regulatory applications in the European Union. Following the authorization, Merck received another feather in its cap. The company has always been a pioneer in developing breakthrough medications that control the global pandemic. The life-saving medication will not only save the life of COVID-19 patients, but also be an effective oral therapeutic for lung disorders. This is a major boost to COVID-19 treatment, which included only vaccines as a preventive measure.
The phase 3 clinical trial of molnupiravir was known as MOVe-OUT clinical trial. The positive results of this clinical trial compelled the authorities to give a positive feedback. In this trial, 800 mg of molnupiravir was administered orally to COVID-19 patients who are neither hospitalized nor vaccinated. The medication was given twice daily after laboratory tests confirmed that their symptoms were mild to moderate. These patients had at least one risk factor, such as diabetes and heart disease.
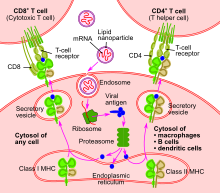
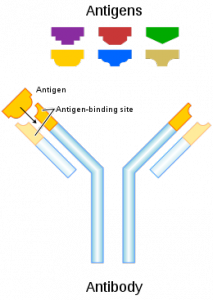
The collaboration between patients and physicians seemed to be successful in this clinical trial. This is an extraordinary effort in controlling the global pandemic. The efforts of all brave volunteers of this clinical trial must be applauded. Merck is now working hard to gain licenses from other global regulatory authorities in order to broaden the access to this wonder drug globally. Let’s understand what is molupiravir in biological terms. Well, it is a potent form of a ribonucleoside, preventing SARS-CoV-2 from replicating and proliferating. This virus is the leading cause of COVID-19.
The efficacy of molnupiravir is now being evaluated in the prophylaxis MOVe-AHEAD study. This phase 3 study would be performed in a randomized, double-blind manner; however, the control would be a placebo and the clinical trial would be in a multicentre setting. The goal is to evaluate whether molnupiravir is effective in controlling and preventing COVID-19 in household patients. The clinical trial patients were not vaccinated for SARS-CoV-2. Moreover, they had at least one underlying disease that could complicate their case of COVID-19.