Kidney cancer is a potentially lethal illness with little hope for cure. At the University of North Carolina, scientists have been trying to explore a new treatment therapy for kidney cancer. The Lineberger Comprehensive Cancer Center is attached to the University of North Carolina.
Scientists working at this institute have developed a potential therapeutic target that can be used for treating kidney cancers; they have been successful in identifying the gene that causes kidney cancer.
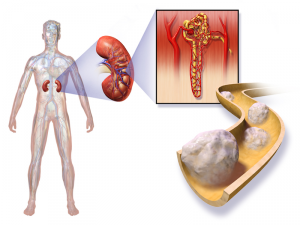
An overabundance of blood vessels leads to tremendous genetic change in patients with kidney cancer. Owing to the excessive flow of blood, tumors are developed easily. This finding is promising enough to be considered as a pathway for the development of cancer in patients.
A genetic change was observed in more than 90 percent of patients, which were diagnosed with the most common type of kidney cancer. It is important to note that VHL is a tumor suppressor gene, which is lost due to a change in genetic conditions.
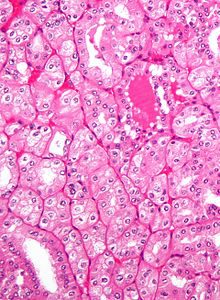
In these cells, there is an over-accumulation of a protein termed as ZHX2. The over-accumulated protein would instigate other signals, which are involved in the growth of cancerous tumors. Based on these findings, we suggest that ZHX2 is potentially a new therapeutic target that is associated with the development of renal cell carcinoma.
Following the suppression of the gene VHL, several ZHX2 proteins would be accumulated in the human body. Consequently, signals related to kidney cancer would be promoted. The expression of this protein must be destroyed in order to treat kidney cancer patients; the therapeutic treatment may be a single drug or combination of drugs.
Genetic mutations or alterations have occurred in more than 90 percent of cases with renal cell carcinoma.In patients with renal cell carcinoma, VHL is the most important gene that suppresses tumor.
Several reports have suggested that VHL plays an important role in every stage of renal cell carcinoma, which includes initiation to tumor progression to metastasis.
It is important to note how kidney cancer would be developed with the loss of function of VHL. In kidney cancer patients, the downstream effects of VHL function loss can be targeted therapeutically.
Several cell signals are involved in the excessive production of blood vessels. There are FDA approved drugs that block these signals, which cause downstream manifestation of VHL protein. This would be the standard mode of treatment for patients with renal cell carcinoma.
Most patients would hardly respond to these drugs. Moreover, these patients would quite often show drug resistance; therefore, researchers wanted to identify other targets that were accumulated in cells that lacked normal functioning of VHL gene. Cancerous cell growth was promoted with the abnormal functioning of VHL gene.
Researchers wanted to understand how oncogenesis is being promoted in kidney cancer cells following the loss of VHL function. A screening technique was created by researchers to identify new molecules, which would be useful in driving cancer cells after the loss of function of VHL.
In kidney cancer cells, the expression of VHL was lacking but the expression of ZHX2 was promoted. From laboratory models, the protein ZHX2 was eliminated completely. With this treatment strategy, the growth of cancer cells would be inhibited. Moreover, metastasis of cancer would also be suppressed effectively.
Several novel therapies have been developed for the treatment of kidney cancer. These therapies are as follows: i) molecular target therapy and ii) treatments based on immunology. However, several novel therapeutic targets must be used to treat metastatic condition in patients with kidney cancer.
Mutated forms of VHL are observed in most patients with kidney cancer; therefore, it is very imperative to investigate this gene. There have been several advancements in kidney cancer treatment modalities in the past few years. More than a dozen drugs have been approved by the FDA for the treatment of kidney cancer.
