Many factors have to be considered while doing right journal selection for your manuscript. Most novice researchers do not know the factors to be considered before submitting the manuscript to a journal. If the journal is not related to the topic of your research, the article would be rejected even without being subjected to peer review process. Now, let us understand which factors need to be considered for journal selection.
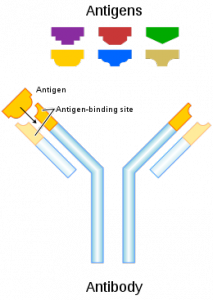
- Topic of research: Each journal has aims and scopes, which should be explored and matched with the topic of research. Suppose a researcher has written an article on novel therapies for lung cancer, then the researcher should submit the paper to a journal whose name and scope is aligned with lung cancer therapy.
- Types of articles: Many journals publish a certain type of article. Full length paper will not be published in a journal that publishes only case study. Moreover, a systematic review would not be appropriate for publication in a journal of manuscripts.
- Journal’s impact factor: Before submitting a paper to a journal, always consider the impact factor of the journal. Greater the impact factor of the journal, higher is the visibility of the article. Papers published in high impact journals usually receive greater citations and credibility.
- Journal’s target audience: The content of the article should be compliant with the target audience of the journal. If an article is about latest medications and therapies, then the article would be read by a clinical journal and not by a chemical journal. There are many interdisciplinary fields of study, such as robotic surgery in bioinformatics. These papers are read by both surgeons and biomedical engineers.
- Length of the article: Most journals have laid down strict wordcount restrictions. In general, most biomedical journals do not want abstracts that are more than 250 words. Similarly, most academic journals accept papers that have a wordcount of 3000-5000 words. A pre-press service author education company should be hired to concise the article and abstract and adhere to wordcount restrictions. These wordcount limits are usually displayed in the “Instructions to Authors” Tab of the journal’s website.
- The type of journal: Science Citation Index (SCI), Open Access (OA), and Hybrid are the three types of journals in academic publishing. The leading publishers are Elsevier, Springer, Nature, Wiley, etc. In general, most Asian researchers publish in SCI journals, while most European researchers prefer to publish in OA journals. Today, hybrid mode of publishing includes the benefits of both SCI and OA journals, so it is now used by researchers all across the world.
Based on these factors, researchers should select three closely related journals for publication of their manuscript.